No waiting at all today at UCH - got right in, vitals and blood drawn and sent off to lab. Short wait for results.
The "white side" of my blood counts (infection fighting) continues to improve upward. My white blood cell count is up to 2.1 (norms 4-11.1), still low, but, much better.
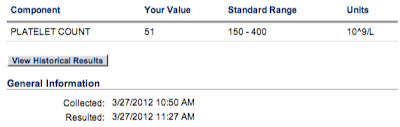
My platelets for clotting are not holding after each platelet transfusion. They were 30 (norms 150-440) today and I'll be getting my 4th platelet transfusion today since the VDT-PACE chemotherapy from Mar 16-20 2012.
The "red side" of my blood counts (oxygen carrying energy cells) continues to drift downward. Today, my hemoglobin was 8.4 (norm 12.1-16.3). No wonder those walks yesterday were a tad hard for me. At any rate, they do not give blood transfusions for low hemoglobin until the value is 8.0 or lower. However, they are anticipating that my hemoglobin will continue its downward trend and they drew blood for a type and cross match to have 2 units of blood ready for me on Monday, April 2 2012.

My Absolute Neutrophil Count (ANC) is coming up and is at 1.7 today (norms 1.8-7.8), so I can almost be in public with a mask on to go someplace like a store.

These next two tests are the type an cross for the potential blood transfusion on Monday, April 2 2012. I have Type A Positive Blood with a Negative Antibody. When you get a blood transfusion, it is important that that match your blood type.
All of my other lab values are normal in my comprehensive metabolic panel.
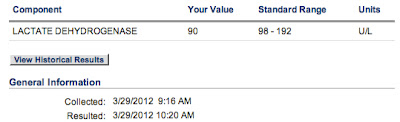
My LDH (inflammation marker) remains low at 94 (norms 98-192).
My Magnesium is normal at 1.8 (norms 1.3-2.10
My Phosphorus is normal at 2.7 (norms 2.7-4.4).
My Uric Acid is normal eat 4.1 (norms 2.6-8.7).
I got my 4th platelet transfusion since my VDT-PACE chemotherapy on Mar 16-20 2012.
- Platelet Transfusion March 24 2012
- Platelet Transfusion March 27 2012
- Platelet Transfusion March 29 2012
- Platelet Transfusion March 31 2012
We were in an out of UCH in record time and home just 4 hours 15 minutes after we left Greeley. Jani says I should write this down someplace, as it usually takes much longer...